In 1855, transmetatarsal amputations (TMA) were originally used to treat trench foot. However, their use has since become widespread by podiatric, vascular, and orthopedic physicians to treat patients with several diagnoses. Diabetic patients (DM) are often a subgroup who receive this level of amputation as an alternative to more proximal amputations. A TMA is an effective procedure to manage severe forefoot infection and ulceration in DM patients because it aims to maximize foot function and energy expenditure by preserving a significant portion of the foot.6 TMAs allow patient ambulation, can maintain a patient’s independence, and can be disguised with normal footwear.
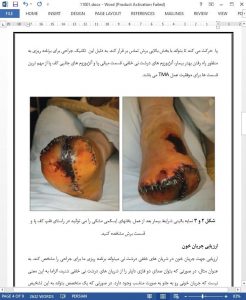
However, research has shown that despite TMAs being a good surgical option for DM patients, many of the recipients tend to experience difficulty with wound closure. Wound breakdown is a common complication that has been shown to occur in 40-70% of TMAs, and 82% of patients who receive TMAs go on to need additional procedures due to complications.5,6 Several theories have been proposed to explain this phenomenon, but none have been accepted as a definitive explanation.