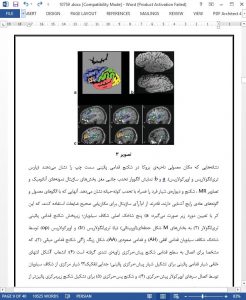
Since the birth of functional magnetic resonance imaging (fMRI)—a noninvasive tool able to visualize brain function—now 15 years ago, several clinical applications have emerged. fMRI follows from the neurovascular coupling between neuronal electrical activity and cerebrovascular physiology that leads to three effects that can contribute to the fMRI signal: an increase in the blood flow velocity, in the blood volume and in the blood oxygenation level. The latter effect, gave the technique the name blood oxygenation level dependent (BOLD) fMRI. One of the major clinical uses is presurgical fMRI in patients with brain abnormalities. The goals of presurgical fMRI are threefold: 1) assessing the risk of neurological deficit that follows a surgical procedure, 2) selecting patients for invasive intraoperative mapping, and 3) guiding of the surgical procedure itself. These are reviewed here. Unfortunately, randomized trials or outcome studies that definitively show benefits to the final outcome of the patient when applying fMRI presurgically have not been performed. Therefore, fMRI has not yet reached the status of clinical acceptance. The final purpose of this article is to define a roadmap of future research and developments in order to tilt pre-surgical fMRI to the status of clinical validity and acceptance.
THE GOAL OF SURGICAL TREATMENT of brain tumors is the complete removal of the abnormality, while minimizing the risk of inducing (permanent) neurological deficits. Resection of primary brain tumors improves survival, functional performance, and the effectiveness of adjuvant therapies, provided that surgicallyinduced neurological deficits can be avoided (1). Therefore, the proposed margin of the surgical resection should not violate functionally eloquent cortical areas. Mapping of these areas is traditionally achieved by invasive methods such as intraoperative cortical stimulation (ICS) in the awake patient, implantation of a subdural grid with extraoperative stimulation mapping, or operative sensory-evoked potential recordings. While accurate, these techniques are rather difficult to perform, place great stress on the awake patient, and often require a larger craniotomy than necessary for the removal of the tumor. Another major disadvantage of these techniques is that a surgical procedure itself is required before any functional information can be obtained. As a result, important patient management decisions must be made without complete knowledge of the anatomic relationship between the lesion borders and functionally eloquent cortex.
CONCLUSIONS
In conclusion, presurgical fMRI in patients with brain tumors is a promising clinical application with added value. In well-trained hands, and realizing its limitations— especially the lack of differentiating essential from expendable brain areas, and reduced or absent fMRI signal that anecdotally occurs in some patients—it allows assessment of the risk of therapeutic interventions, selection of patients for intraoperative mapping, and guides brain surgery itself. However, fMRI has not yet reached the status of clinical acceptance. Combining presurgical fMRI with other techniques such as DTI and TMS should give it that status in the near future.